Fatty liver – symptoms, causes, and digestion
How Livers function ?
The liver is a vital organ in the human body, responsible for a wide range of essential functions. Its primary function is to process nutrients from the food we eat and convert them into energy or store them for later use. The liver plays a crucial role in detoxifying harmful substances, such as drugs and alcohol, from the bloodstream. Additionally, it produces bile, which aids in the digestion and absorption of fats in the small intestine. The liver also regulates blood sugar levels by storing excess glucose as glycogen and releasing it when needed. Moreover, it synthesizes proteins necessary for blood clotting and immune system function. Overall, the liver’s multifaceted functions are indispensable for maintaining overall health and well-being.
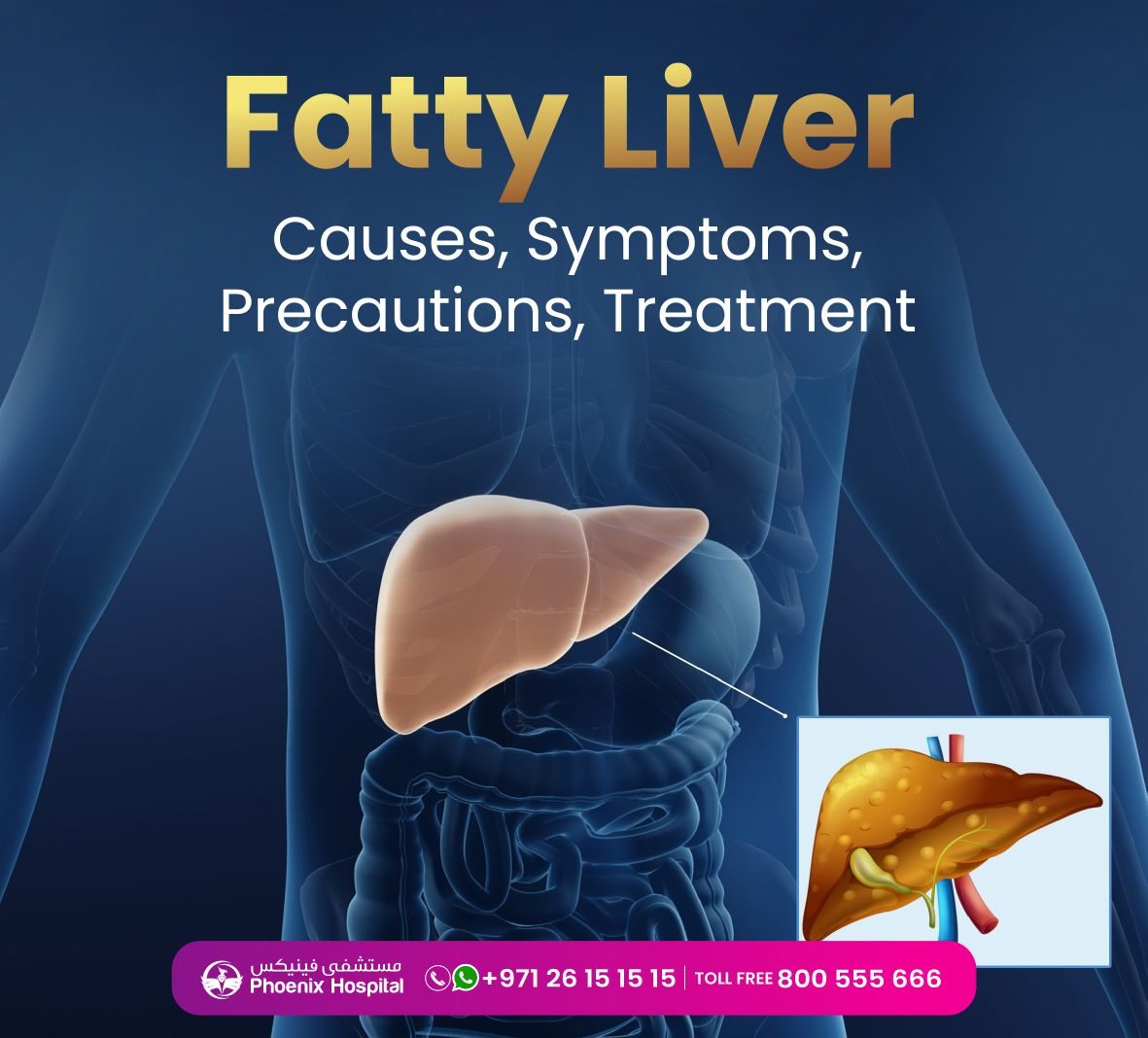
What is fatty liver?
Fatty liver, medically known as hepatic steatosis, is a condition where triglycerides accumulate within the liver cells, causing it to become enlarged and heavier. This build-up of fat is often associated with factors such as obesity, high cholesterol, diabetes, and excessive alcohol consumption. The two primary types of fatty liver are alcoholic fatty liver disease (AFLD) and non-alcoholic fatty liver disease (NAFLD). NAFLD is more common and not related to excessive alcohol intake.
Types of fatty liver
• NAFLD- Non Alcoholic fatty liver Disease
• AFLD- Alcoholic Fatty liver
• Non-Alcoholic Fatty Liver Disease (NAFLD): NAFLD is the most common type of fatty liver and occurs in individuals who do not consume excessive alcohol. It is often associated with conditions like obesity, insulin resistance, type 2 diabetes, high cholesterol, and metabolic syndrome. NAFLD can range from simple fatty liver, where there is an accumulation of fat in the liver cells, to non-alcoholic steatohepatitis (NASH), a more severe form with inflammation and liver cell damage.
• Alcoholic Fatty Liver Disease (AFLD): AFLD is caused by excessive alcohol consumption over a prolonged period. The liver is responsible for metabolizing alcohol, and excessive intake can lead to the buildup of fat in the liver cells. AFLD can progress to more severe conditions like alcoholic hepatitis and cirrhosis if alcohol consumption continues.
Stages of fatty liver
• Simple fatty liver: In the early stages of fatty liver disease, there is an accumulation of fat in the liver cells, but there is hardly to no inflammation or liver cell damage. At this stage, the condition is usually asymptomatic, and it may not cause any noticeable health issues. However, it’s essential to detect and address this stage to prevent its progression.
• Steatohepatitis: As the disease advances, it can progress to NASH, which involves inflammation and liver cell damage in addition to the accumulation of fat. NASH is more concerning than simple steatosis because it can lead to more severe liver complications, such as fibrosis (scarring of the liver tissue). NASH may cause symptoms like fatigue, abdominal discomfort, and elevated liver enzyme levels in blood tests.
• Fibrosis: Continued inflammation and liver cell damage can lead to the development of fibrosis. Fibrosis is the formation of scar tissue in the liver, which can affect liver function and impede blood flow through the organ. The extent of fibrosis determines the severity of the condition, and advanced fibrosis may progress to cirrhosis.
• Cirrhosis: Cirrhosis is the most severe stage of fatty liver disease. At this point, there is extensive scarring of the liver tissue, which disrupts normal liver function. Cirrhosis can lead to liver failure, where the liver is unable to perform its vital functions adequately. This stage may manifest with symptoms like jaundice, fluid retention, confusion, and an increased risk of bleeding and infections.
• Hepatocellular Carcinoma: Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, which means it originates in the liver itself rather than spreading to the liver from another location. HCC typically develops in the hepatocytes, which are the main functional cells of the liver.
Why liver health depends on what we eat ?
Liver health is closely tied to what we eat because the liver plays a central role in processing and metabolizing the nutrients and substances we consume. The liver acts as a filter, processing everything that enters our body through the digestive system, including food, beverages, and medications. Here are several reasons why liver health depends on what we eat:
• Nutrient Metabolism
• Detoxification
• Fat Processing
• Regulation of blood sugar
• Protein synthesis
• Antioxidant Support
• Weight management
Why liver become fatty liver
• Obesity
• Unhealthy Diet
• Insulin resistance
• Type 2 Diabetes
• High Cholesterol and Triglycerides
• Excessive alcohol consumption
• Metabolic syndrome
• Rapid Weight loss
• Certain Medications
• Genetics
Symptoms
• Abdominal pain upper right side
• Fluid accumulation in abdomen
• Tummy fat
• Jaundice
• Loosing weigh without intention
• Muscle wasting
• Abdominal bleeding
• Spider veins (angioma)
• Hepatic encephalopathy
• Urine & stool changes
• Men’s breast enlargements
• Dilated veins
• Low thyroid
Self-precaution
Maintaining liver health and preventing fatty liver disease is crucial for maintaining liver health and preventing fatty liver disease. Here are some critical self-precautions to consider:
• Maintain a Healthy Diet: Adopt a balanced and nutritious diet that includes fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods, sugary beverages, and foods high in saturated and Tran’s fats.
• Manage Weight: Maintain a healthy weight through a balanced diet and regular exercise. Obesity is a significant risk factor for fatty liver disease, so achieving and maintaining a healthy weight is essential.
• Limit Alcohol Consumption: Drink alcohol in moderation. Excessive alcohol consumption is a leading cause of alcoholic fatty liver disease. For women, moderate drinking is defined as up to one drink per day, and for men, up to two drinks per day.
• Exercise Regularly: Engage in regular physical activity to support overall health and promote liver function. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, along with muscle-strengthening exercises on two or more days per week.
• Avoid smoking: Smoking harms the liver and impair its function. If you smoke, consider quitting to reduce liver-related complications.
• Manage Diabetes and Blood Pressure: If you have diabetes or high blood pressure, work with your healthcare provider to manage these conditions effectively. Properly controlling blood sugar and blood pressure levels can protect the liver.
• Stay Hydrated: Drink plenty of water throughout the day to support overall organ function, including the liver.
• Limit Medication Use: Be cautious with over-the-counter medications and avoid the unnecessary use of potentially harmful medications. Always follow prescribed dosages and consult your healthcare provider if you have concerns about medication interactions.
• Check for Hepatitis Infections: Hepatitis B and C infections can cause liver damage. If you are at risk or unsure of your vaccination status, consider getting tested and vaccinated.
• Manage Stress: Chronic stress can affect overall health, including liver health. Practice stress-reduction techniques such as meditation, yoga, or spending time doing activities you enjoy.
• Regular Check-ups: Schedule regular check-ups with your healthcare provider to monitor your liver health and address any potential concerns promptly.
“In Phoenix Hospital, our team of professional doctors and staffs are ready to help and deliver you the best possible care. It’s always good to take a second opinion, Our experienced doctors are willing to help you with your healthcare decisions. You can get in touch with us by clicking contact
You can also Schedule an appointment with our doctors through Book an Appointment”